Improving palliative care in ICUs with telemedicine - Research project launched under Charité leadership
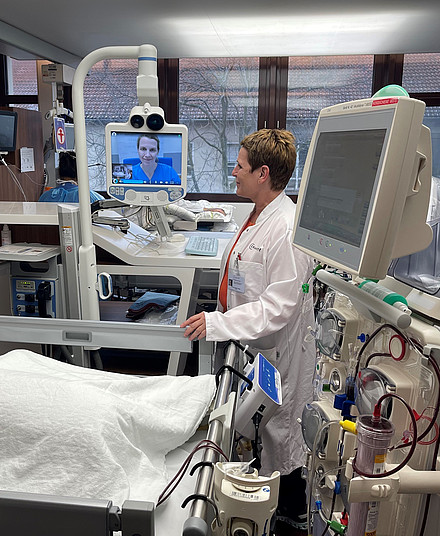

Alleviating pain and other symptoms for seriously ill patients to preserve and support their remaining lifespans and quality of life is the goal of palliative medicine. It is an important and established part of intensive care. However, if the patient’s disease and symptoms are very complex, it can be helpful for ICU staff to turn to palliative medicine specialists for advice on specific cases. “But not every hospital has in-house expertise in palliative medicine,” says Prof. Claudia Spies, Director of the Department of Anesthesiology and Intensive Care Medicine at Charité. “Systematic use of telemedicine that allows experts to be brought in virtually, and thus fast and from anywhere, could bring even more improvement in the palliative care provided in ICU settings.”
A practical model with three strands: continuing education, checklists, telemedicine
So how much benefit do telemedicine consultations with palliative medicine experts bring in comparison to the palliative care typically provided in an intensive care unit? A team of researchers is working to answer that question in the EPIC project. “Before the telemedicine consultation phase starts, the ICU clinical staff will first receive training in palliative medicine,” explains Spies, who is heading up the research project. “We’re also working on checklists to help the teams identify the patients who could benefit from specialized palliative care as early as possible.” Some 2,000 patients and their families are participating in the research project, which is being carried out at seven clinical centers with palliative medicine and 23 multidisciplinary ICUs in five European countries.
“EPIC is bringing together clinicians and researchers from the areas of palliative and intensive care, social sciences, nursing, ethics, and health economics with the goal of implementing a harmonized practical model of palliative care at ICUs, and not just in one country, but all across Europe,” Spies explains. “We hope our project will help us identify recommended actions that we can pass along to specialized organizations and that can be included in initial and continuing education and training for the next generation of intensive care staff across multiple professions.”
Shorter ICU stays
Studies show that integrating palliative medicine as soon as possible shortens the amount of time patients spend in intensive care, although mortality remains the same. With this in mind, one of the researchers’ goals in EPIC is to reduce the time patients spend in the ICU – which not only has benefits from a health economics standpoint, but is also of immeasurable value for the patients themselves. “When patients with severe and incurable diseases receive optimum palliative care, then they hopefully won’t have to spend their last days in the ICU, unless there’s a very serious reason. This can be a blessing for them and their families during this extremely critical and highly vulnerable phase at the end of life,” Spies says. “And palliative care is also helpful for people with severe or chronic disease who are not approaching the end of life. People often confuse palliative medicine with hospice, but they aren’t the same. About half of patients can be discharged and go home with specialized palliative treatment. So improving palliative care across the board would benefit all of the patients in the ICU.”
Another of the researchers’ aims in EPIC is to study how well patients and family members respond to palliative medicine that is provided with telemedicine support. They also plan to establish a group for patients and families to share their stories and information and provide mutual support.
About EPIC
The research consortium is headed up by Prof. Claudia Spies, Director of the Department of Anesthesiology and Intensive Care Medicine on Campus Charité Mitte and Campus Virchow-Klinikum. Funding is being provided as part of the EU’s Horizon Europe framework program. The other partners in the consortium are: General University Hospital in Prague (Czech Republic), Hebrew University of Jerusalem (Israel), Heinrich-Heine-Universität Düsseldorf (Germany), King’s College Hospital (United Kingdom), KU Leuven (Belgium), Martin Luther University Halle-Wittenberg (Germany), the Faculty of Medicine of the University of Basel (Switzerland), National and Kapodistrian University of Athens (Greece), Università degli Studi di Perugia (Italy), the University of Southern Denmark (Denmark), Universitätsklinikum Erlangen (Germany), the European Association for Palliative Care (Belgium), the European Society of Anaesthesiology and Intensive Care (Belgium), and tp21 GmbH (Germany). There are plans to start a cooperation with a group representing patients and families.



